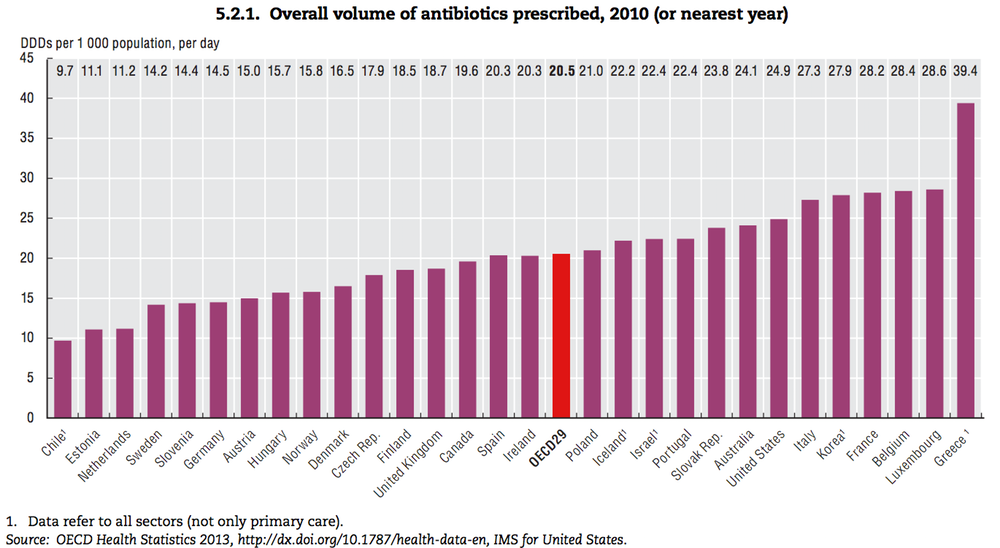
Antibiotic prescription rate differs across countries. It is two times greater in Korea than in Norway (27.9 vs. 15.8: Defined Daily Doses (DDDs) per 1000 people per day, 2015 OECD report). Why are antibiotics over prescribed in Korea?
One reason might be that it is difficult to find traditional medicines in Korean market. In contrast, Norwegians can buy a FLU SHOT at convenience stores. It is a bitter version of Jamba Juice. It is filled with traditional medicines such as ginger, turmeric, garlic, and cayenne pepper.



If I can buy the same FLU SHOT in Korea, I may not need to see doctors often. My thought provides fresh insights into behavioral economists. In the past, how to nudge doctors not to prescribe antibiotics was studied. Now, how to nudge patients not to see doctors may need to be studied.
Reference
Meeker, Daniella, Jeffrey A. Linder, Craig R. Fox, Mark W. Friedberg, Stephen D. Persell, Noah J. Goldstein, Tara K. Knight, Joel W. Hay, Jason N. Doctor (2016), “Effect of Behavioral Interventions on Inappropriate Antibiotic Prescribing Among Primary Care Practices: A Randomized Clinical Trial,” Journal of the American Medical Association, 315 (6), 562-570.
IMPORTANCE: Interventions based on behavioral science might reduce inappropriate antibiotic prescribing.
OBJECTIVE: To assess effects of behavioral interventions and rates of inappropriate (not guideline-concordant) antibiotic prescribing during ambulatory visits for acute respiratory tract infections.
DESIGN, SETTING, AND PARTICIPANTS: Cluster randomized clinical trial conducted among 47 primary care practices in Boston and Los Angeles. Participants were 248 enrolled clinicians randomized to receive 0, 1, 2, or 3 interventions for 18 months. All clinicians received education on antibiotic prescribing guidelines on enrollment. Interventions began between November 1, 2011, and October 1, 2012. Follow-up for the latest-starting sites ended on April 1, 2014. Adult patients with comorbidities and concomitant infections were excluded.
INTERVENTIONS: Three behavioral interventions, implemented alone or in combination: suggested alternatives presented electronic order sets suggesting nonantibiotic treatments; accountable justification prompted clinicians to enter free-text justifications for prescribing antibiotics into patients’ electronic health records; peer comparison sent emails to clinicians that compared their antibiotic prescribing rates with those of “top performers” (those with the lowest inappropriate prescribing rates).
MAIN OUTCOMES AND MEASURES: Antibiotic prescribing rates for visits with antibiotic-inappropriate diagnoses (nonspecific upper respiratory tract infections, acute bronchitis, and influenza) from 18 months preintervention to 18 months afterward, adjusting each intervention’s effects for co-occurring interventions and preintervention trends, with random effects for practices and clinicians.
RESULTS: There were 14,753 visits (mean patient age, 47 years; 69% women) for antibiotic-inappropriate acute respiratory tract infections during the baseline period and 16,959 visits (mean patient age, 48 years; 67% women) during the intervention period. Mean antibiotic prescribing rates decreased from 24.1% at intervention start to 13.1% at intervention month 18 (absolute difference, -11.0%) for control practices; from 22.1% to 6.1% (absolute difference, -16.0%) for suggested alternatives (difference in differences, -5.0% [95% CI, -7.8% to 0.1%]; P = .66 for differences in trajectories); from 23.2% to 5.2% (absolute difference, -18.1%) for accountable justification (difference in differences, -7.0% [95% CI, -9.1% to -2.9%]; P < .001); and from 19.9% to 3.7% (absolute difference, -16.3%) for peer comparison (difference in differences, -5.2% [95% CI, -6.9% to -1.6%]; P < .001). There were no statistically significant interactions (neither synergy nor interference) between interventions.
CONCLUSIONS AND RELEVANCE: Among primary care practices, the use of accountable justification and peer comparison as behavioral interventions resulted in lower rates of inappropriate antibiotic prescribing for acute respiratory tract infections.

